
Moderate quality evidence suggests having subthreshold symptoms of mania, emotional dysregulation, or behaviour problems are also associated with greater likelihood of switching to mania in children with major depression. Moderate to high quality evidence finds having a positive family history of any mood disorder is associated with greater likelihood of switching to mania in children with major depression. Most of the time, bipolar disorder symptoms start during late adolescence or early adulthood. Odd appearance, grandiosity, flight of ideas, decreased sleep, and increased sexual interest are more common in adults with bipolar disorder. Some people have hypomanic episodes, which are like manic episodes, but not severe enough to cause marked impairment in social or occupational functioning or require hospitalization. Moderate to high quality evidence finds irritability, aggression, and low insight are more common in youths than adults with bipolar disorder.
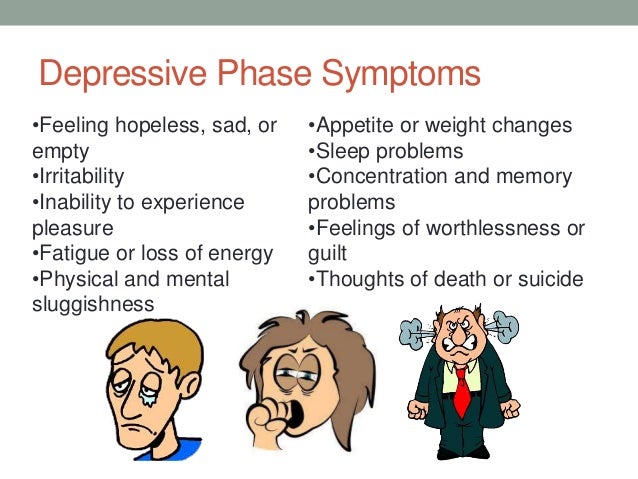
Moderate quality evidence finds the most common mania symptoms reported in youths with bipolar disorder are (in decreasing order) increased energy, irritability, mood lability, distractibility, goal-directed activity, euphoric/elated mood, pressured speech, hyperactivity, racing thoughts, poor judgment, grandiosity, inappropriate laughter, decreased need for sleep, and flight of ideas. What is the evidence for mania symptoms in bipolar disorder? The frequency and severity of manic or hypomanic symptoms vary from person to person, and may also vary according to whether the onset of bipolar disorder is in childhood, adolescence, or adulthood. Hypomanic symptoms do not lead to the major problems that mania often causes, and the person is still able to function. A hypomanic episode is similar to a manic episode but the symptoms are less severe and need only last four days in a row. These changes in behaviour are significant and clear to friends and family and are severe enough to cause major dysfunction. A manic episode involves changes in normal behaviour, including showing exaggerated self-esteem or grandiosity, less need for sleep, talking more than usual, talking more loudly and quickly, being easily distracted, doing many activities at once, scheduling more events in a day than can be accomplished, embarking on risky behaviour, uncontrollable racing thoughts, and/or quickly changing ideas or topics. When you become depressed, you may feel sad or hopeless and lose interest or pleasure in most activities. doi:10.What are mania symptoms in bipolar disorder?Ī manic episode is a period of at least one week when a person is high spirited or irritable in an extreme way most of the day for most days. Bipolar disorder, formerly called manic depression, is a mental health condition that causes extreme mood swings that include emotional highs (mania or hypomania) and lows (depression). The manic behaviors, thoughts, or moods occur most of the day or nearly every day in that period. Bipolar disorder diagnosis: challenges and future directions. In people with bipolar 1 disorder, manic episodes last at least 7 days. Prevalence and treatment of panic disorder in bipolar disorder: systematic review and meta-analysis. Preti A, Vrublevska J, Veroniki AA, Huedo-Medina TB, Kyriazis O, Fountoulakis KN. Recognizing binge-eating disorder in the clinical setting: A review of the literature. Kornstein SG, Kunovac JL, Herman BK, Culpepper L. Antidepressants in bipolar depression: an enduring controversy. Borderline personality disorder and bipolar disorder: what is the difference and why does it matter?.

Overdiagnosis of bipolar disorder: a critical analysis of the literature. Ghouse AA, Sanches M, Zunta-Soares G, Swann AC, Soares JC. Treatment of cyclothymic disorder: commentary. Depression and pain: often together but still a clinical challenge: a review.

Clinical and demographic features associated with the detection of early warning signs in bipolar disorder. The diagnosis and treatment of bipolar disorder: decision-making in primary care.


 0 kommentar(er)
0 kommentar(er)
